If you have tried submitting insurance claims for Applied Behavior Analysis therapy, you may be familiar with ABA therapy billing.
This particular type of billing process helps service providers and patients in ABA therapy submit claims to insurance companies when they need it.
However, the need for a different billing method that includes special codes may raise a few eyebrows. This article will help address any questions or concerns you may be harbouring.
We will explore what ABA billing is and why it is needed in the healthcare industry. More importantly, we will also demonstrate how this form of billing can help you mitigate legal risks submitting claims to insurance companies.
What is ABA Billing in Healthcare?
Applied Behavior Analysis (ABA) billing is a billing method used by people and certain sectors in healthcare. Generally, it is related to ABA therapy billing services for treating autism and other behavioral issues.
In this form of treatment or therapy, specialists use a structured approach to help patients improve their social, communication, and learning skill
The question of billing is essential here because ABA therapy billing is often covered by insurance. To this end, healthcare professionals must follow certain billing practices.
ABA billing has strict guidelines set by insurance companies. These are aligned with healthcare regulations. For instance, it involves submitting claims that will accurately reflect the services provided by the therapists.
As mentioned earlier, there are certain billing codes specific to this form of billing. The ABA billing codes help insurers understand the duration and type of ABA therapy billing the patient received. Additionally, it outlines the therapist or service provider’s qualifications.
ABA billing requires detailed documentation of the whole therapy process. This attention to detail ensures both parties have a clear understanding of the medical necessities.
Furthermore, this ensures that patients can get the care that they need. It also ensures that the patients have no cause for concern regarding the denial of their claims by insurance companies or any resulting and unnecessary delays.
Legal Risks of Traditional Healthcare Billing
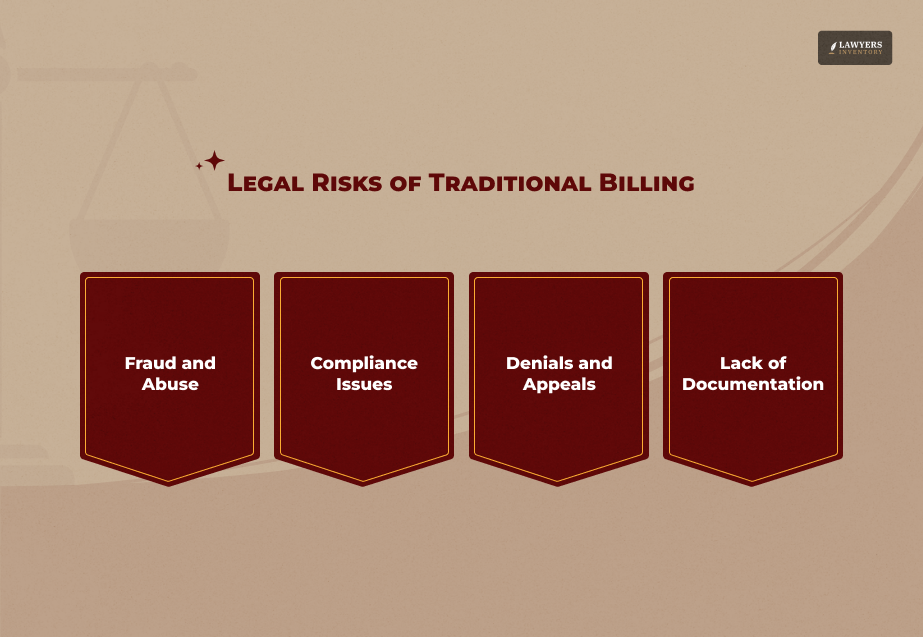
“But why does a simple billing need to be made complicated?”
A more studied assessment reveals that traditional billing systems have several pitfalls that could cause legal trouble for patients seeking this therapy.
For instance, if service providers do not follow the billing rules or specific guidelines for a condition, several legal consequences that can arise.
For example, you could face financial penalties, loss of medical license, and other legal actions.
Here are some of the legal risks of traditional billing in healthcare that you should be aware of:
1. Fraud and Abuse
Firstly, traditional billing systems and practices can be vulnerable to fraud and abuse, in the form of monetary extortion. This is probably one of the most significant legal concerns in the healthcare industry today.
According to the National Health Care Anti-Fraud Association (NHCAA), the United States suffers from healthcare fraud costs of about $68 billion annually.
But why and when does this happen? It generally occurs when service providers submit a false claim related to their services. In such a case, they usually charge for a service they have not provided.
These types of fraud can be either intentional (billing for an expensive product instead of a basic one) or unintentional (entering incorrect billing codes by mistake).
Regardless, the government takes these matters seriously as evidenced by laws like the False Claims Act. If law enforcement catches an ABA service provider submitting a false claim, they will face legal consequences.
2. Compliance Issues
Secondly, there are people in the healthcare industry who do not follow strict billing systems or guidelines. In other words, they do not comply with the regulations of the governing body.
Failure to comply with these laws will result in audits, fines, and the inability to bill insurance companies. According to a 2023 CMS report, over 12% of claims were denied due to non-compliance issues.
Compliance issues usually arise because providers do not keep up with the changes in healthcare laws. For instance, insurance companies and government programs like Medicare and Medicaid update their billing policies frequently.
If the service providers use outdated billing codes and fail to follow the new rules, the insurance companies will automatically deny their claims. This results in financial and legal issues.
3. Denials and Appeals
Thirdly, traditional billing methods in healthcare are a mixture of appeals and denials. The cycle is an almost endless one.
For instance, insurance companies reject claims if they find a lack of documentation. And if the claim is denied, the providers will have to go through the tedious process of making an appeal. This is not only time-consuming but also expensive.
If the government or the insurance company suspects that the service provider has been submitting incorrect claims, they will launch an investigation. The matter may escalate from such circumstances.
4. Lack of Documentation
Finally, there is the lack of documentation. This is one of the major drawbacks that most people do not consider initially. When it comes to billing in healthcare, proper documentation is vital.
If the service provider fails to supply the proper documents for the treatment and ABA therapy billing that they have provided, insurance companies will refuse to pay for the services. This will ultimately result in financial losses that could have easily been avoided.
Apart from losing money, not having medical documentation could also lead to legal consequences. For instance, if an audit is undertaken and the provider fails to provide the document, he or she might have to face charges of financial fraud.
ABA Billing: Can It Mitigate the Legal Risks?
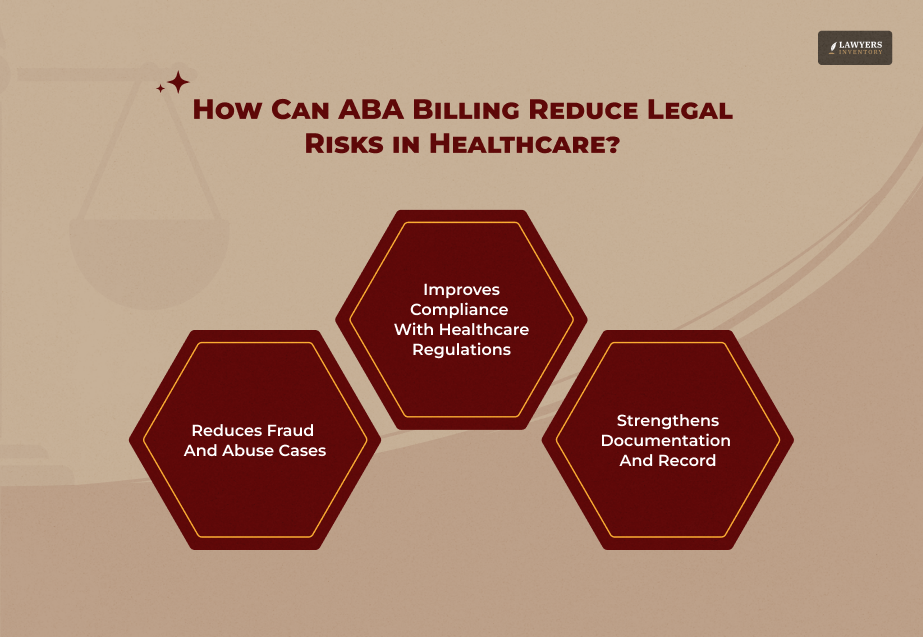
Now that you know how traditional billing methods in healthcare might not be ideal when dealing with Applied Behavior Analysis or ABA therapy, we’ll address how to reduce these risks.
ABA billing helps mitigate risks significantly. This billing method ensures transparency, accuracy, and compliance.
Following an approach that is structured helps minimize the chances of denials, frauds, as well as other legal penalties.
Here’s how ABA therapy billing helps mitigate these risks:
1. Reducing Fraud and Abuse Cases
As ABA therapy Billing follows standardized coding and requires detailed documentation, it reduces the chances of fraud significantly.
Additionally, this is a great way for healthcare providers to protect themselves from accusations of fraud and incorrect billing. Eventually, this helps you to stay away from penalties under the False Claims Act.
2. Improving Compliance with Healthcare Regulations
Secondly, ABA billing ensures that you comply with the regulations and rules of the healthcare programs. It aligns with HIPAA, Medicaid, and other legal requirements and ensures that service providers submit claims correctly.
3. Minimizing Claim Denials and Appeals
Thirdly, ABA therapy billing includes a thorough process of keeping the record through medical documents and audits. Thus, when providers or patients submit their initial claims, they can avoid lengthy denial and appeal cycles.
This method is streamlined and structured. It not only saves time but is naturally more cost-efficient.
4. Strengthening Documentation and Record-Keeping
Finally, as mentioned above, inadequate documentation can result in providers facing accusations of improper billing and legal scrutiny.
For instance, the Office of Inspector General (OIG) has identified poor record-keeping as a key factor in many billing fraud investigations. This is something that you can avoid through ABA billing.
Considering that you need to follow the specific codes of ABA billing methods, it is virtually impossible to miss out on any information that needs documentation.
Best Practices for Implementing ABA Billing
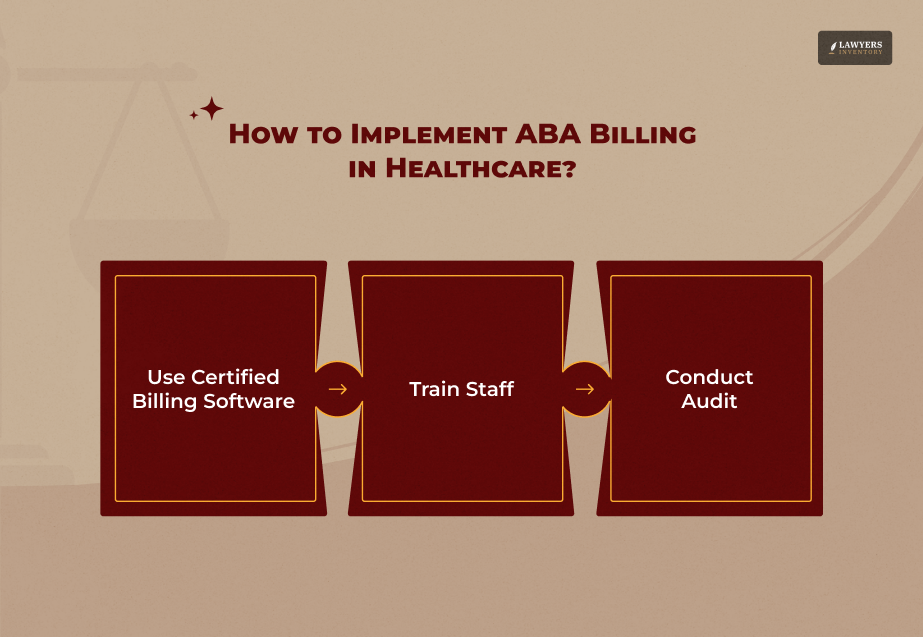
If you are planning to get the maximum benefit of using ABA therapy billing methods, there are a few things that you can do. Here are some of them:
1. Use Certified Billing Software
Firstly, it is essential that you use billing machines and authentic software. According to a 2022 Black Book Market Research survey, 82% of healthcare providers who used automated billing software reported fewer claim denials and billing errors.
This is something that you can avoid with proper billing machines. Ultimately, it will also reduce the chances of legal complications in the future.
2. Train Staff
Secondly, we all know that getting into a habit requires training and practice. This is why you must ensure that staff is trained to handle ABA therapy billing machines and codes efficiently.
Furthermore, this is a great way to reduce mistakes. It will also help them stay updated with regulation changes.
3. Conduct Audit
Lastly, in order to avoid any legal conflicts later,, it is best to conduct regular audits.
You must review billing records, claims, and documentation at regular intervals. This is the best way to ensure compliance with legal and insurance requirements.
Read Also:
- Questions to Ask a Lawyer Before You Sign Them For Your Case
- Understanding Wrongful Death Lawsuits: A Guide For Families
- How to Get a Debt Lawsuit Dismissed in the FASTEST Way!











0 Reply
No comments yet.